Heart-Healthy Diet to Control Insulin Spikes
A CardioNatural “steady energy, steady arteries” guide for smoother blood sugar, lower cravings, and better cardiometabolic health.
This article is for education only and isn’t medical advice. If you take diabetes medications (including insulin), blood thinners, or have kidney disease, talk with your clinician before making major diet or exercise changes. Some links may be affiliate links; if you buy through them, CardioNatural may earn a small commission at no extra cost to you.
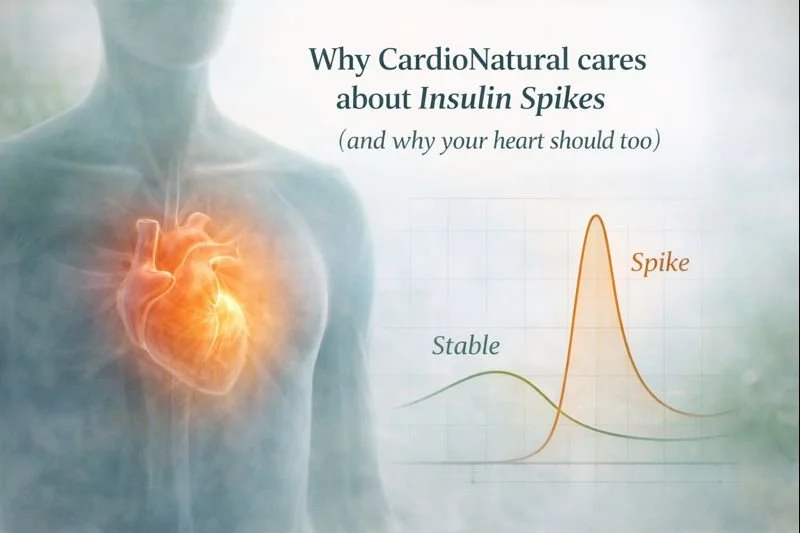
Why CardioNatural cares about insulin spikes (and why your heart should too)
Insulin is the hormone that helps move glucose (blood sugar) from your bloodstream into your cells for energy. When you eat—especially refined carbs or sugary foods—blood sugar can rise quickly. Your body answers with a bigger insulin release to bring glucose down.
That “up-and-down” cycle matters for your heart because metabolic dysfunction (insulin resistance, prediabetes, diabetes, metabolic syndrome) is strongly tied to cardiovascular risk. The American Heart Association notes diabetes as a major controllable risk factor for cardiovascular disease. www.heart.org The AHA also describes metabolic syndrome (often driven by insulin resistance) as a condition that raises risk of heart disease and diabetes. www.heart.org
Even if you don’t have diabetes, frequent large spikes can keep you on a rollercoaster of:
cravings → overeating → weight gain
higher triglycerides (especially after meals)
fatigue/brain fog
…and over time, more insulin resistance.
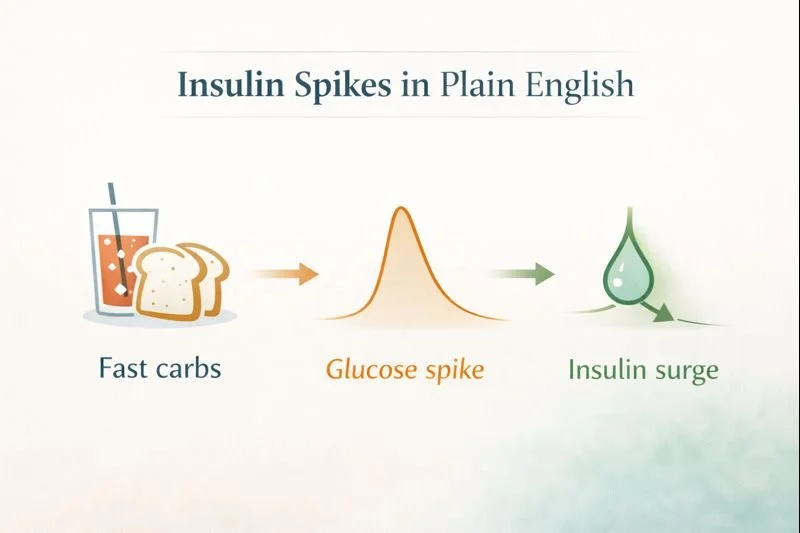
“Insulin spikes” explained in plain English
What causes a spike?
A spike is most often triggered by rapidly absorbed carbohydrates (think: sweet drinks, white bread, pastries, chips, many cereals). The faster glucose rises, the more insulin your body tends to release.
Why spikes can be worse after 35–40 (or after a heart event)
As we age (and especially with stress, poor sleep, inactivity, belly fat, or certain meds), insulin sensitivity often declines. The AHA lists physical inactivity and insulin resistance among underlying causes related to metabolic syndrome. www.heart.org
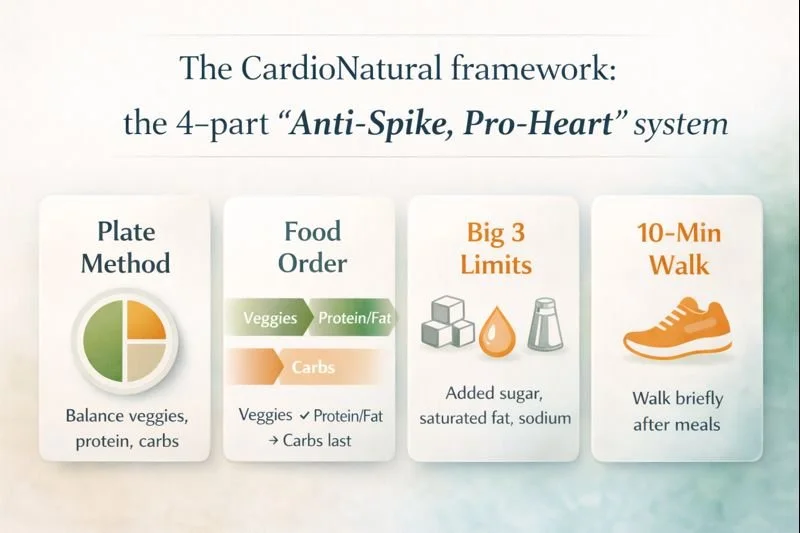
The CardioNatural framework: the 4-part “Anti-Spike, Pro-Heart” system
If you do nothing else, do these four. They cover “every aspect” without turning your life into a math class.
1) Build meals using the Diabetes Plate Method (simple, powerful)
The American Diabetes Association’s updated “Plan Your Plate” tool uses a 9-inch plate:
½ plate: non-starchy vegetables
¼ plate: lean protein
¼ plate: quality carbohydrates
Plus water/low-calorie beverages. American Diabetes Association+1
Why it works: It automatically reduces “carb overload,” increases fiber and protein, and improves fullness—without obsessing over numbers.
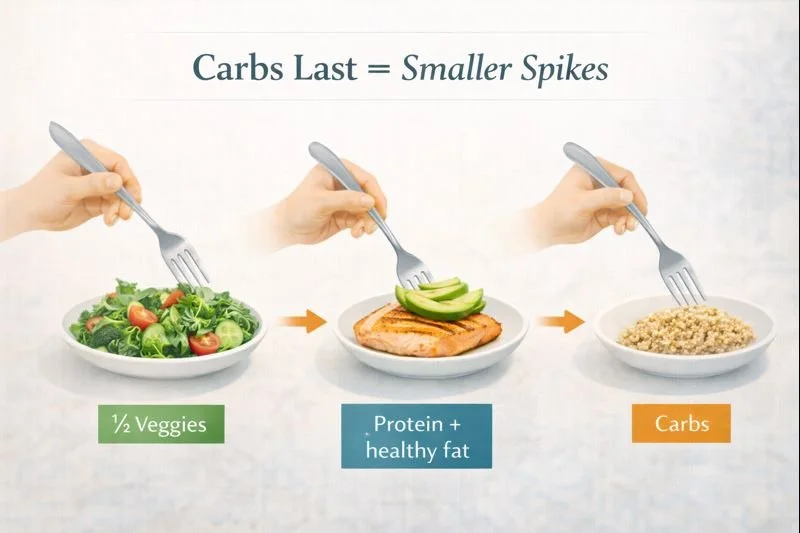
2) Control spikes by food order (yes—order matters)
A surprisingly effective tactic is simply eating:
Veggies/fiber first
Protein + healthy fat next
Carbs last
Research reviews and trials show that eating carbs last (after vegetables/protein) can reduce post-meal glucose and insulin excursions. PMC+2PMC+2
Try this today:
Start every lunch/dinner with a salad, veggie soup, or a big serving of non-starchy veggies before touching rice, bread, or dessert.
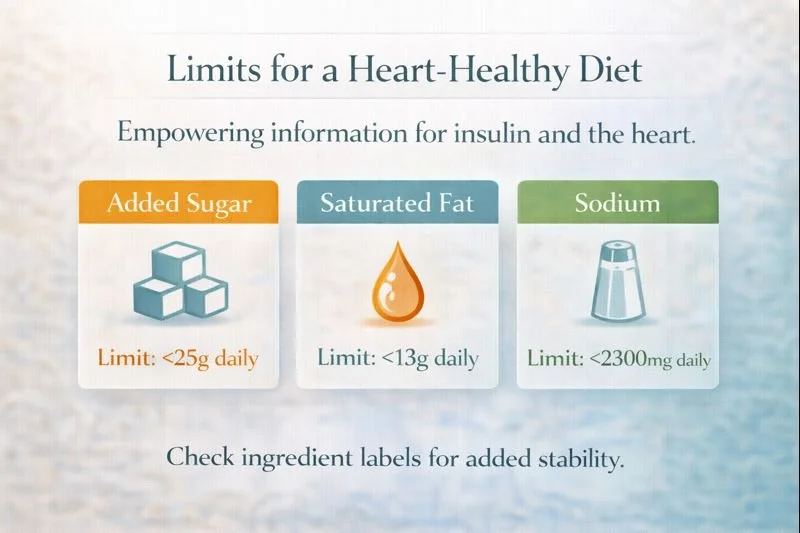
3) Pick heart-healthy fats (and be strict with the “big 3” limits)
For cardiometabolic health, the AHA emphasizes an overall pattern rich in plants, whole grains, and healthy proteins—and minimizing added sugar and saturated fat. www.heart.org+1
AHA targets you can actually use:
Added sugar: AHA recommends limiting added sugars to no more than 6% of calories/day (often summarized as ~6 tsp women, ~9 tsp men). www.heart.org
Saturated fat: AHA recommends <6% of total calories from saturated fat. www.heart.org
Sodium: AHA recommends ≤2,300 mg/day, with an ideal goal of 1,500 mg/day for most adults. www.heart.org
Why this matters for insulin spikes: high-sugar, high-saturated-fat, high-sodium ultra-processed foods are often “triple threats” for blood sugar, appetite, and blood pressure.
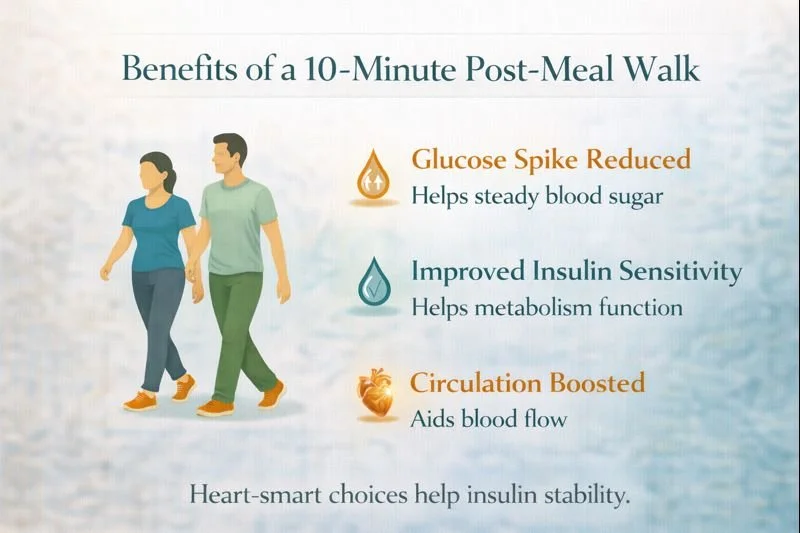
4) Use the “10-minute after-meal walk” to blunt peaks
A 2025 study found a brief 10-minute walk immediately after a meal lowered peak glucose compared with doing nothing. PMC+1
This is one of the simplest “free hacks” that works with real life.
Also, general activity targets matter: the CDC’s National DPP lifestyle approach includes increasing activity to at least 150 minutes/week. CDC+1
The best heart-healthy foods for steadier insulin
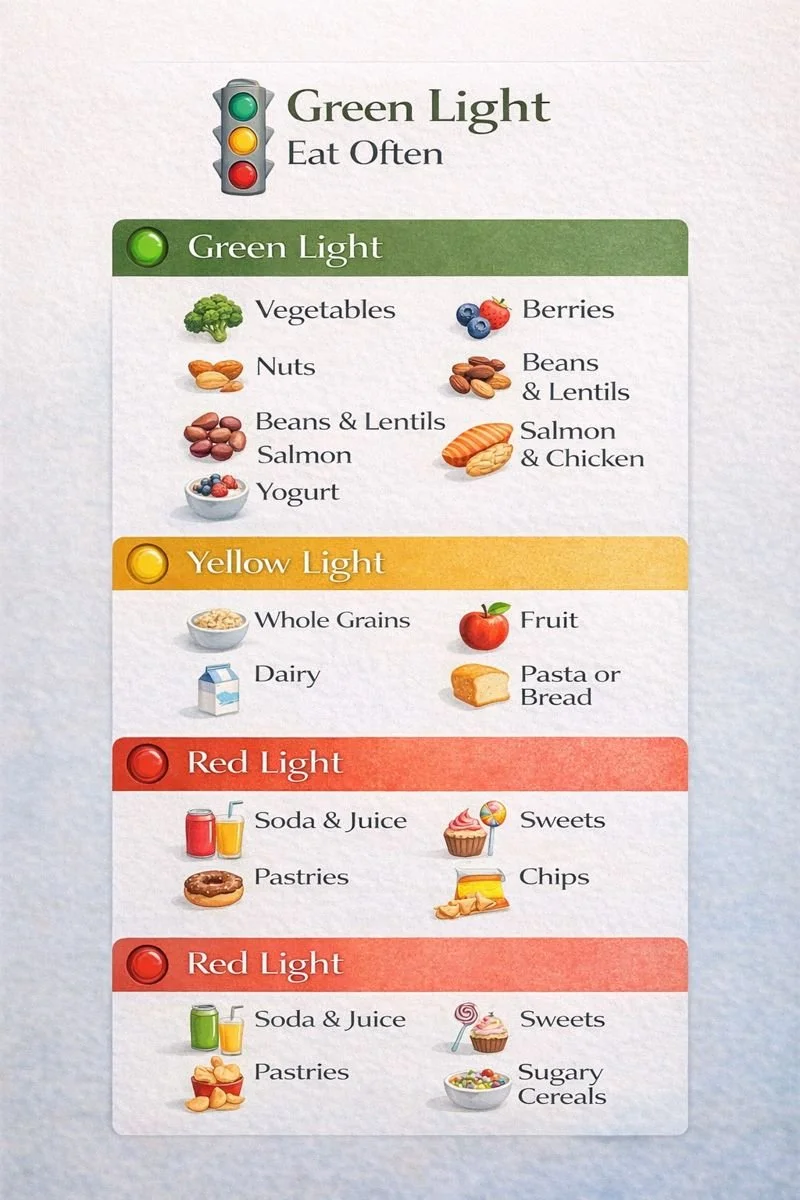
Your “Green Light” list (eat often)
Non-starchy vegetables (unlimited-ish):
Leafy greens, broccoli, cauliflower, peppers, mushrooms, zucchini, asparagus.
Proteins (aim every meal):
Fish/seafood, chicken/turkey, eggs, Greek yogurt/cottage cheese, tofu/tempeh, beans/lentils (also carbs, but “smart carbs”).
Smart carbs (portion-controlled):
Beans/lentils, oats, quinoa/barley, berries, apples/pears, citrus, sweet potato, plain yogurt/kefir.
Fats (the heart winners):
Extra-virgin olive oil, avocado, nuts, seeds (chia/flax), olives.
Why fiber is a superstar: Higher fiber intake is linked with lower cardiometabolic risk, and meta-analytic evidence suggests increases in fiber are associated with reduced cardiovascular disease risk. PMC+1
The “yellow light” foods (not banned—just strategic)
Whole-grain bread, brown rice, whole-wheat pasta (keep portions modest; carbs-last order)
Fruit (choose whole fruit; pair with protein/fat)
Dark chocolate (small portion; pair with nuts)
The “red light” spike-starters (limit hard)
Sugary drinks, juice, sweet coffee drinks
Pastries, candy, most desserts
White bread, many crackers/chips, highly refined cereal
“Low-fat” flavored yogurts (often sugar-heavy)
Giant bowls of rice/pasta without protein + veg
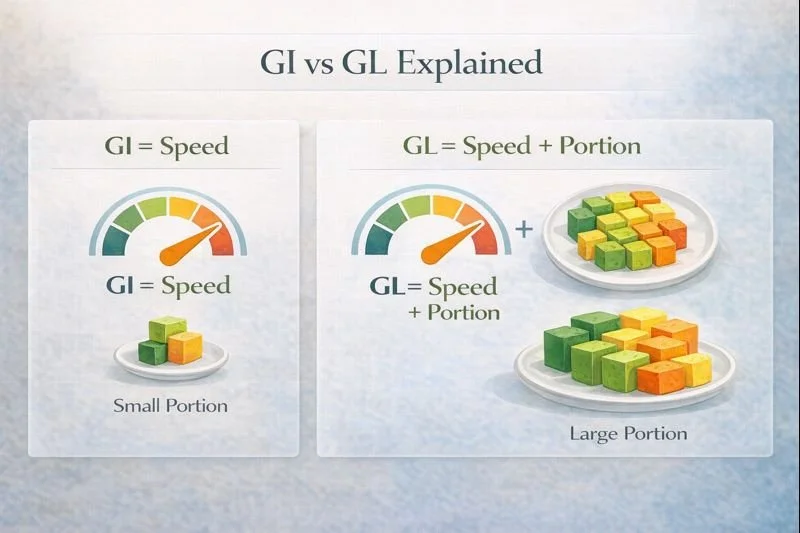
Carb quality matters: GI/GL in real life (without the confusion)
Glycemic Index (GI) ranks how quickly a carb-containing food raises blood sugar; glycemic load (GL) accounts for both GI and portion size. EatrightPRO+1
In plain English: portion + processing matter as much as the food itself.
Practical use (CardioNatural style):
Don’t chase “perfect GI.”
Instead: choose minimally processed carbs, keep portions reasonable, and always pair with protein/fiber/fat.
Your CardioNatural “Anti-Spike Plate” templates
Template A: The default lunch/dinner plate (ADA-inspired)
½ plate: roasted/steamed veggies or big salad
¼ plate: protein (fish/chicken/tofu/beans)
¼ plate: quality carbs (beans, quinoa, sweet potato, fruit) American Diabetes Association+1
Fat: 1–2 tbsp olive oil or a small handful of nuts/seeds
Template B: The “breakfast that doesn’t spike you”
Protein: 25–35g
Fiber: 8–12g
Carbs: mostly berries/oats/seed-based
Examples:Greek yogurt + berries + chia + walnuts
Veggie omelet + avocado + side berries
Protein smoothie (unsweetened) + chia/flax + spinach + berries
Template C: The “snack that prevents a crash”
Aim: protein-forward + fiber
Apple + peanut butter
Cottage cheese + cinnamon + berries
Hummus + veggies
Greek yogurt + nuts
Meal timing: does it matter?
For most people, what matters most is:
consistent meals
less late-night ultra-processed eating
walking after meals
If evenings are your worst spike window, make dinner your lowest refined-carb meal and lean heavier on veggies + protein.
The movement plan that stabilizes insulin and protects your heart
Minimum effective plan
After meals: 10 minutes walking PMC+1
Weekly: target 150 minutes/week of moderate activity CDC+1
Add strength training: helps muscles store/use glucose better (bonus for aging well). Evidence reviews support aerobic + resistance training for glycemic control. PMC
If you’re busy:
Do 10 minutes after your biggest meal + 2 short strength sessions/week. That’s still a game-changer.
A content-heavy 7-day CardioNatural meal plan (heart-healthy + anti-spike)
Use carbs-last order at every lunch/dinner.
Day 1
Breakfast: Greek yogurt + berries + chia + walnuts
Lunch: Salmon salad + chickpeas (½ cup)
Dinner: Chicken/tempeh stir-fry + mixed veggies + quinoa (½–¾ cup cooked)
Optional snack: Apple + nut butter
Day 2
Breakfast: Eggs + spinach + 1 slice whole-grain toast
Lunch: Lentil soup + side salad
Dinner: Cod + Brussels sprouts + small sweet potato
Snack: Cottage cheese + cinnamon
Day 3
Breakfast: Oats + chia + blueberries + added protein (Greek yogurt or protein powder)
Lunch: Turkey or tofu lettuce wraps + avocado + veggie sticks
Dinner: Turkey chili (beans + veggies) + broccoli
Snack: Almonds + dark chocolate (small)
Day 4
Breakfast: Smoothie (unsweetened protein + spinach + berries + flax/chia)
Lunch: Tuna/salmon salad over greens + fruit
Dinner: Sheet-pan chicken/tofu + veggies + quinoa
Snack: Hummus + carrots/celery
Day 5
Breakfast: Avocado + smoked salmon on whole-grain (portion-controlled)
Lunch: Mediterranean bowl (chicken + veggies + olives + feta + farro OR cauliflower rice)
Dinner: Shrimp + veggie sauté + cauliflower rice
Snack: Pear + pistachios
Day 6
Breakfast: Chia pudding + berries + pumpkin seeds
Lunch: Black bean veggie salad + grilled protein
Dinner: Lean steak/tempeh + asparagus + roasted cauliflower + beans (½ cup)
Snack: Greek yogurt + cocoa + raspberries
Day 7
Breakfast: Veggie omelet + berries
Lunch: Sardines/salmon + whole-grain crackers (portion) + big salad
Dinner: Whole-wheat pasta (¾ cup cooked) + marinara + extra veggies + chicken/white beans
Snack: Cheese stick + cucumber
Want a more “program-like” approach? You can rotate Days 1–3 repeatedly and swap proteins/veggies.
Grocery list (anti-spike staples)
Produce: greens, broccoli, cauliflower, peppers, cucumbers, tomatoes, zucchini, berries, apples/pears, citrus, onions, garlic
Proteins: salmon/sardines/tuna, chicken/turkey, eggs, Greek yogurt, cottage cheese, tofu/tempeh
Carbs (smart): lentils, beans, chickpeas, oats, quinoa, barley/farro, sweet potatoes
Fats: extra-virgin olive oil, avocados, walnuts/almonds, chia/flax, pumpkin seeds
Flavor: cinnamon, turmeric, vinegar, herbs, lemon/lime
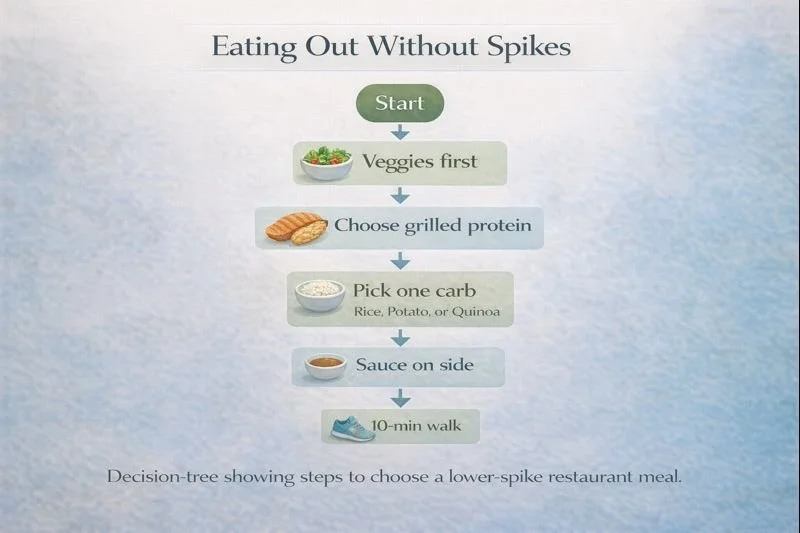
Eating out without spikes (real-world guide)
Order veggies first (salad, steamed veg, veggie soup).
Choose grilled protein.
Pick one carb: beans, small potato, small rice, or fruit.
Ask for sauces on the side; use olive oil/lemon if possible.
Take a 10-minute walk after. PMC+1
Troubleshooting: if you’re “doing everything right” but still spiking
1) Hidden sugar + refined carbs
Look at drinks, sauces, “healthy” snacks, and breakfast items.
2) Portions are sneaky
Even healthy carbs can spike if the portion is large. Reduce carb portion slightly and increase veggies/protein.
3) Sleep and stress are the silent spike multipliers
Short sleep and chronic stress can worsen insulin resistance for many people—work on routine and wind-down.
4) You may be in CKM territory (heart–kidney–metabolic overlap)
The AHA has highlighted cardiovascular-kidney-metabolic (CKM) syndrome as a connected risk framework—meaning blood sugar, blood pressure, cholesterol, kidney markers, weight, sleep, and lifestyle work as a system. www.heart.org
Special safety notes (important)
If you take insulin or sulfonylureas: changing carbs + walking after meals can drop glucose—coordinate with your clinician.
If you’re on warfarin: leafy greens aren’t “bad,” but keep vitamin K intake consistent and follow your clinician’s guidance.
If you have kidney disease: potassium/phosphorus/sodium targets may differ—get individualized advice. (Also note AHA sodium targets for most adults.) www.heart.org
Quick-start checklist (print this)
Use the ADA Plate Method for lunch/dinner. American Diabetes Association+1
Eat veggies → protein/fat → carbs last. PMC+2PMC+2
Keep added sugar, saturated fat, sodium in AHA ranges. www.heart.org+2www.heart.org+2
Walk 10 minutes after meals. PMC+1
Aim for 150 minutes/week movement as your baseline. CDC+1