How to Naturally Prevent (and Sometimes Reduce) Plaque Buildup in Arteries — What Actually Works
Important note (Cardio Natural style): If you have chest pain, shortness of breath, one-sided weakness, slurred speech, or new/worsening symptoms, treat that as urgent medical care. This article is education—not a substitute for your clinician. If you already have known plaque, prior stents, a heart attack, or stroke/TIA, lifestyle is still powerful—but it should be added to (not used to replace) proven medical care.
People often ask, “How do I remove plaque naturally?”
Here’s the truth: the body can sometimes shrink certain plaque types a little, especially when the causes are aggressively reversed (high LDL/ApoB, high blood pressure, smoking, insulin resistance, chronic inflammation). But the bigger win—and what saves lives—is that you can slow plaque growth, stabilize it (make it less likely to rupture), and dramatically lower event risk through evidence-based “natural” levers.
This post will show you exactly what to do.
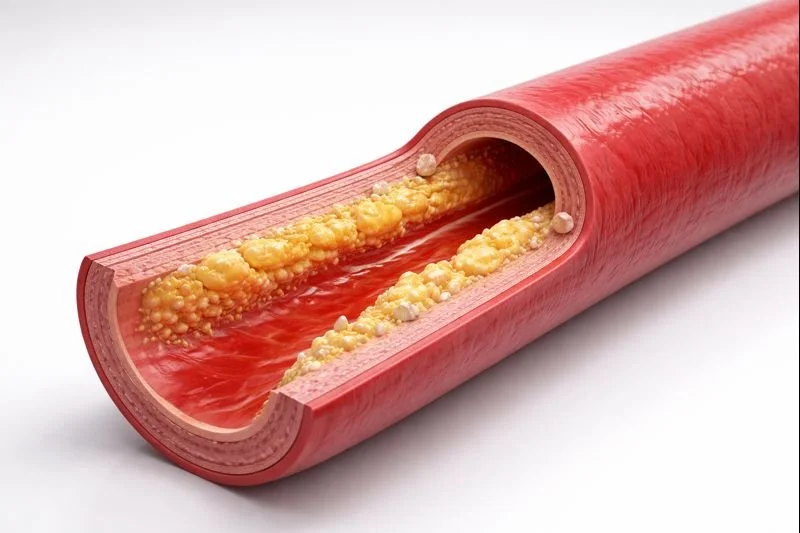
What “plaque” really is (and why “clogging” is only part of the story)
Artery plaque (atherosclerosis) isn’t just “cholesterol stuck to a pipe.” It’s a living, inflammatory process inside the artery wall. Plaque can include:
LDL-cholesterol particles and immune cells
scar tissue (“fibrous cap”)
calcium (older, more stable plaque)
inflammatory components (higher risk if the cap is thin)
Most heart attacks happen when a plaque ruptures, not when an artery is 95% blocked. A smaller, inflamed plaque can be more dangerous than a larger, stable one.
So the goal is:
Lower the raw material that builds plaque (ApoB/LDL particles)
Reduce artery-wall injury (blood pressure, smoking, glucose swings)
Calm inflammation and strengthen the fibrous cap (exercise, sleep, diet pattern)
The “Big 5” natural levers that move plaque the most
If you only focus on five things, focus here—these align with major heart guidelines and lifestyle recommendations. AHA Journals+2www.heart.org+2
1) Lower LDL (and ideally ApoB): the #1 plaque lever
LDL/ApoB particles are the delivery trucks that deposit cholesterol into the artery wall. Lowering them reduces progression and event risk.
Food moves LDL. Meds can be needed too, but your “natural” baseline matters a lot.
Key diet targets the AHA emphasizes:
Limit saturated fat (AHA suggests <6% of calories) and avoid trans fats www.heart.org
Build meals around plants + fiber (vegetables, legumes, whole grains, nuts, seeds) www.heart.org+1
2) Control blood pressure: less “wear-and-tear” on artery walls
High BP injures the inner lining of arteries, making it easier for plaque to form and harder to stabilize. Lifestyle changes (activity, sodium reduction, weight, sleep) are core AHA recommendations. www.heart.org+1
3) Stop smoking (including “just a little”)
Smoking accelerates plaque growth and destabilizes plaques. If you do one thing for your arteries fast—this is it. (AHA lifestyle guidance consistently puts smoking at the top.) www.heart.org+1
4) Improve insulin sensitivity (blood sugar & triglycerides)
Insulin resistance increases triglycerides, small dense LDL, inflammation, and endothelial dysfunction. You don’t need perfection—you need trend improvement (food pattern, strength training, walking, sleep).
5) Move daily: exercise stabilizes plaque
Exercise improves blood pressure, insulin sensitivity, triglycerides, and vascular function. AHA commonly recommends ~150 minutes/week moderate (or equivalent) for heart health. www.heart.org+1
Can plaque actually shrink with lifestyle alone?
Sometimes, modestly—especially with intensive lifestyle changes. Classic trials led by Dean Ornish showed that comprehensive, high-adherence lifestyle programs could produce measurable regression in coronary atherosclerosis in some participants. JAMA Network+2PubMed+2
Two important nuances:
These programs were intensive (diet pattern, stress management, activity, support).
Even when plaque doesn’t shrink dramatically, risk can fall a lot because plaque becomes more stable and inflammation drops.
So yes—“natural regression” can happen, but the reliable promise is: stabilize + slow + reduce risk.
The Cardio Natural Anti-Plaque Food Framework (practical + realistic)
The best “default” pattern: Mediterranean-style (with a plant-forward tilt)
A Mediterranean-style eating pattern has strong evidence for cardiovascular risk reduction and is repeatedly endorsed in heart-health guidance. The PREDIMED trial (and its later republication/reanalysis) supported benefits of a Mediterranean pattern supplemented with extra-virgin olive oil or nuts. New England Journal of Medicine+1
Your plate most days:
½ plate non-starchy vegetables (color variety)
¼ plate protein (fish, legumes, tofu/tempeh, poultry; red meat less often)
¼ plate high-fiber carbs (beans, lentils, oats, quinoa, barley, sweet potato)
Add healthy fat (extra-virgin olive oil, nuts, seeds, avocado)
The 4 foods that quietly “de-plaque” your bloodwork (by lowering LDL)
These don’t sound exciting, but they work because they lower LDL/ApoB drivers.
Soluble fiber (daily)
Oats, barley (beta-glucan), beans/lentils, chia/flax, apples/citrus
Soluble fiber is associated with LDL reduction; psyllium supplementation has evidence for LDL improvements. AHA Journals+2NCBI+2
Nuts (most days)
A small handful (walnuts, almonds, pistachios)
Extra-virgin olive oil
Use as main cooking fat (not tropical oils as your default)
Legumes (4–7x/week)
Beans/lentils are “LDL-lowering + glucose-stabilizing + filling”
Saturated fat: the plaque “accelerator” most people underestimate
You don’t need to fear fat—you need to choose fats that don’t raise LDL.
Common high-saturated-fat traps:
butter, heavy cream, high-fat cheese
fatty red meats, processed meats
many ultra-processed foods
AHA’s guidance to limit saturated fat is specifically aimed at cholesterol reduction. www.heart.org+1
The 30-day “Stop Plaque in Its Tracks” plan (simple, not perfect)
Daily non-negotiables (takes ~30–45 minutes total)
10-minute walk after 2 meals (breakfast and/or dinner works)
One “fiber anchor”: oats or beans or psyllium (more below)
One big salad or veggie bowl (at least 3 colors)
Protein at each meal (keeps cravings down, supports muscle)
Sleep window: choose a consistent “lights out” target
This aligns with the AHA concept that foundational lifestyle habits drive risk down across multiple pathways. www.heart.org+1
Weekly structure
2–3 strength sessions/week (even 20 minutes: push/pull/squat/hinge/core)
150 minutes/week moderate cardio (brisk walking counts) www.heart.org+1
Plan 3 “home base” meals you repeat (repetition beats willpower)
Supplements: what’s worth considering (and what’s mostly hype)
Food-first always. Supplements can help specific lab targets, but they rarely outperform the lifestyle fundamentals.
1) Psyllium husk (soluble fiber)
Best for: LDL reduction, better regularity, improved satiety
Evidence: fiber (including psyllium) is linked to LDL improvements. AHA Journals+2NCBI+2
How to use (typical approach): start low, increase gradually, drink water.
2) Plant sterols/stanols
Best for: LDL reduction (especially if your diet is already decent)
Evidence: plant sterols/stanols commonly reduce LDL by ~5–15% in studies; dose-response is reported in reviews and meta-analyses. PMC+2MDPI+2
Common target used in studies: around ~2 g/day.
3) Omega-3s: food first; prescriptions are different than typical fish oil
Best for: triglycerides (and in certain high-risk cases, outcomes with prescription EPA)
Important nuance: Over-the-counter fish oil results differ from prescription-grade EPA used in major outcome studies (like REDUCE-IT). AHA Journals+2American College of Cardiology+2
Practical: aim for fatty fish 2x/week as a baseline, unless your clinician advises otherwise.
Supplements to be cautious with
“Antioxidant megadoses” for heart prevention: USPSTF recommends against vitamin E and beta-carotene for preventing CVD/cancer, and finds evidence insufficient for most other supplements for prevention. USPSTF+2USPSTF+2
“Plaque cleanses” / chelation claims / miracle drops: usually marketing, not medicine.
The inflammation + stress piece (the most ignored plaque stabilizer)
Chronic stress doesn’t just “feel bad”—it can drive:
higher BP
worse sleep
worse food choices
higher inflammation
In intensive lifestyle programs that showed regression signals, stress management and support were part of the intervention, not optional. JAMA Network+1
Cardio Natural practical version (10 minutes/day):
5 minutes slow breathing (long exhale)
5 minutes journaling: “What’s my next right step today?”
What to track (so you know it’s working)
Ask your clinician which labs and targets make sense for you, but commonly useful:
LDL-C (and ideally ApoB if available)
Triglycerides
Blood pressure (home readings)
A1c / fasting glucose (insulin resistance trend)
Waist circumference (a simple proxy for visceral fat)
Lifestyle changes are far more motivating when you can see numbers move.
FAQ
“Can I dissolve plaque naturally?”
You can often reduce the drivers (LDL/ApoB, BP, insulin resistance, smoking) and stabilize plaque, lowering your risk meaningfully. True “plaque reversal” can occur in some people with intensive lifestyle, but it’s not the most reliable promise. JAMA Network+1
“What’s the fastest way to stop plaque from getting worse?”
Stop smoking www.heart.org
Lower saturated fat + increase soluble fiber www.heart.org+1
Walk daily + strength train weekly www.heart.org
Treat BP seriously Mayo Clinic
“If I eat ‘clean,’ do I still need meds?”
Some people do, some don’t. If you have established disease or high risk, guidelines support lifestyle for everyone and add medications when needed to reduce events. AHA Journals+1
Lifestyle is never wasted—it makes meds work better and often allows lower doses.
Your “Cardio Natural” takeaway
If you want the simplest winning formula:
Fiber + plants + olive oil + daily walking + strength training + sleep + no smoking
…and keep lowering what builds plaque (LDL/ApoB) while calming what destabilizes it (BP, glucose swings, inflammation).